Social Determinants of Health
Research overview
Social, economic, and behavioral factors can influence the trajectory of one’s health so significantly they have been coined the “social determinants of health” or SDoH. Those factors include:
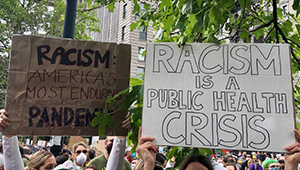
- Personal characteristics such as race, ethnicity, culture, sex, gender identity, and sexual preference
- Economic resources such as educational attainment, employment, income, wealth, and housing
- Built environment such as transportation systems, access to healthy foods, and walkability
- Adverse experiences such as childhood trauma, interpersonal violence, relationship disruption, or bereavement
Researchers at Kaiser Permanente Washington Health Research Institute (KPWHRI) are committed to understanding how the health care system can best identify, understand, and appropriately respond to these factors to improve the health of our members and our communities.
“Through our evaluation and research, we hope to help empower patients to better manage the social and behavioral factors that influence their health,” said Clarissa Hsu, PhD, KPWHRI associate investigator.
Our institute researchers have long been interested in SDoH. Examples include our work in areas such as tobacco addiction and the integration of treatment for behavioral health issues into primary care. We’ve worked on efforts such as reducing racial disparities in care, opioid overuse, and vaccine hesitancy. Our Center for Community Health and Evaluation has helped to promote and sustain healthy communities; our Center for Accelerating Care Transformation (formerly known as the MacColl Center for Health Care Innovation) has championed the Chronic Care Model and has been committed to helping U.S. primary care practices — including community health centers — integrate community resources into health improvement.
Moving forward, we intend to make targeted improvements in the lives of Kaiser Permanente members, but, as these examples suggest, we also work in communities around the nation for broad impact. Here are just a few examples of KPWHRI’s current work related to SDoH:
- Moving to Health
This project is designed to pinpoint what matters most about individual neighborhoods for their residents’ health. Funded by the National Institute of Diabetes and Digestive and Kidney Diseases, researchers will track individuals and the built environment in their neighborhoods to see how changing communities affects factors such as people’s long-term weight and blood sugar — and whether they develop diabetes.
- LINCC (Learning to Integrate Neighborhoods and Clinic Care)
Researchers on this project, funded by the Patient-Centered Outcomes Research Institute, are testing how adding a community resource specialist role in primary care can help connect people with community resources that support health and wellness.
- Team-based opioid management
The goal of this project is to improve safe prescribing and chronic opioid medication for patients with non-cancer pain in rural primary care clinics across Washington and Idaho. Led by KPWHRI’s Center for Accelerating Care Transformation (ACT Center), the project is helping clinics develop policies, workflows, registries, tool kits, and other resources to better support patients with chronic pain. The work is funded by the Agency for Healthcare Research and Quality.
- Addressing financial hardship
In projects funded by the Robert Wood Johnson Foundation, a team of KPWHRI researchers is learning how health care systems can do a better job of talking transparently with patients about the cost and value of their health care. The goal is to help identify “best practices” for making tools and resources part of regular workflows in clinics. Doing so could ultimately help patients have a better understanding of what their care will cost — information that’s important for helping individuals make informed decisions about treatment based on their own values.
KPWHRI researchers are committed to gaining a holistic understanding of people’s lives — one that can best inform prevention, intervention, and implementation efforts, maximizing the public health impact of our efforts.
KPWHRI researchers have a unique constellation of methodological strengths — including qualitative analysis, implementation science, and experience with evidence reviews, evaluation design and methods, measurement development, big data analysis for community intervention evaluation, pragmatic trials, user-centered design, survey research, and community-based participatory research. These strengths are coupled with substantive expertise (for example, nutrition, physical activity, behavioral health, economic and racial disparities, prevention and health promotion, child health and development, and stigma), and a multi-disciplinary, team-science-based approach that is needed to tackle these “thorny issues.”
We hope to realize the optimal role of the health care system in addressing social, economic, and behavioral needs, and partner with the community to create much needed change.
Recent publications on Social Determinants of Health
Mackey CD, Schultz ME, Nguyen KH, Mettert KD, Bernabe AM, Garcia M, Jaffe AE, Larimer ME. A longitudinal investigation of PTSD symptoms, hazardous drinking, and relationship satisfaction in college student dating relationships. J Soc Pers Relat. 2024 Oct;41(10):2983-3007. doi: 10.1177/02654075241259106. Epub 2024 Jun 7. PubMed
McAteer S, Wartko P, Hajat A, Fuller S, Shortreed SM, Butler A, Enquobahrie DA, Garcia R, Dublin S. Racial and ethnic disparities in the incidence and treatment: of urinary tract infection during pregnancy. J Womens Health (Larchmt). 2025 Apr 29. doi: 10.1089/jwh.2024.0940. Online ahead of print. PubMed
Bojkov E, Papajorgji-Taylor D, Paolino AR, Dorsey CN, Barnes KA, Brown MC. Lessons learned on social health integration:Evaluating a novel social health integration and social risk-informed care online continuing professional development course for primary care providers. BMC Med Educ. 2025 Apr 8;25(1):496. doi: 10.1186/s12909-025-06971-9. PubMed
Grasset L, Bis JC, Frenzel S, Kojis D, Simino J, Yaqub A, Beiser A, Berr C, Bressler J, Bülow R, DeCarli CS, Fohner AE, Harrington LB, Helmer C, Ikram MA, Lemaitre RN, Lopez OL, Longstreth WT, Odden MC, Palta P, Schmidt CO, Talluri R, Vernooij MW, Völzke H, Voortman T, Whalen Q, Wittfeld K, Gabe HJ, Mosley TH, Psaty BM, Wolters FJ, Seshadri S, Dufouil C. Selected social and lifestyle correlates of brain health markers: the Cross-Cohort Collaboration. Alzheimers Dement. 2025 Apr;21(4):e70148. doi: 10.1002/alz.70148. PubMed
Mahmud A, Brown MC, Wong ES, Ornelas IJ, Wellman R, Pardee R, Mun S, Singer A, Westbrook E, Barnes K, Haan HD, Lewis CC. Comparison of clinic-based assistance versus a centralized call center on patient-reported social needs: Findings from a randomized pilot social health integration program. BMC Public Health. 2025 Mar 28;25(1):1171. doi: 10.1186/s12889-025-22334-x. PubMed
Mahmud A, Wong ES, Lewis CC, Ornelas IJ, Wellman R, Pardee R, Mun S, Piccorelli A, Westbrook EO, Haan HD, Brown MC. Differences in healthcare utilization across 2 social health support modalities: Results from a randomized pilot evaluation. AJPM Focus. 2025 Feb 15;4(3):100323. doi: 10.1016/j.focus.2025.100323. eCollection 2025 Jun. PubMed
Llamocca EN, Ahmedani BK, Lockhart E, Beck AL, Lynch FL, Negriff SL, Rossom RC, Sanchez K, Sterling SA, Stults C, Waring SC, Harry ML, Yu H, Madziwa LT, Simon GE. Use of ICD-10-CM codes for adverse social determinants of health across health systems. Psychiatr Serv. 2024 Sep 23:appips20240148. doi: 10.1176/appi.ps.20240148. [Epub ahead of print]. PubMed
Grant RW, McCloskey JK, Uratsu CS, Ranatunga D, Ralston JD, Bayliss EA, Sofrygin O. Predicting self-reported social risk in medically complex adults using electronic health data. Med Care. 2024 Jun 4. doi:10.1097/MLR.0000000000002021. [Epub ahead of print]. PubMed
Researchers in Social Determinants of Health
 Clarissa Hsu, PhDAssociate Investigator |
 Katharine A. Bradley, MD, MPHSenior Investigator |
 Claire Allen, MPHManager, Collaborative Science |
 Paula Lozano, MD, MPHSenior Investigator; Director, ACT Center |
 David E. Arterburn, MD, MPHSenior Investigator |
 Joseph E. Glass, PhD, MSWSenior Investigator |
 Beverly B. Green, MD, MPHSenior Investigator |
 Allen Cheadle, PhDSenior Investigator, KPWHRI; Senior Research Associate, CCHE |
 Paula R. Blasi, MPHSenior Collaborative Scientist |
 Gwen Lapham, PhD, MPH, MSWAssistant Investigator |
 Marlaine Figueroa Gray, PhDAssistant Investigator |
 Gregory E. Simon, MD, MPHSenior Investigator |
 Andrea J. Cook, PhDSenior Biostatistics Investigator |
 Dori E. Rosenberg, PhD, MPHSenior Investigator |
 Jennifer F. Bobb, PhDAssociate Biostatistics Investigator |
 Robert Penfold, PhDSenior Investigator |
 Leah K. Hamilton, PhDSenior Collaborative Scientist |
 Jess Mogk, MPHCollaborative Scientist |
 Morgan Justice, MACollaborative Scientist |
 Nicole M. Gatto, PhD, MPHPrincipal Collaborative Scientist |
 Kelsey Stefanik-Guizlo, MPHCollaborative Scientist |
 Theresa E. Matson, PhD, MPHCollaborative Scientist |
 Meagan C. Brown, PhD, MPHAssistant Investigator |
 Linda K. McEvoy, PhDSenior Investigator |
 Kimberly Arthur, MPHCollaborative Scientist |
 Nora Henrikson, PhD, MPHAssociate Investigator |
 Lily N. Shapiro, PhDCollaborative Scientist |
Affiliate researcher
Emily Williams, PhD, MPH
University of Washington School of Public Health