Do mast cells hold the key to chronic and unexplained disease?
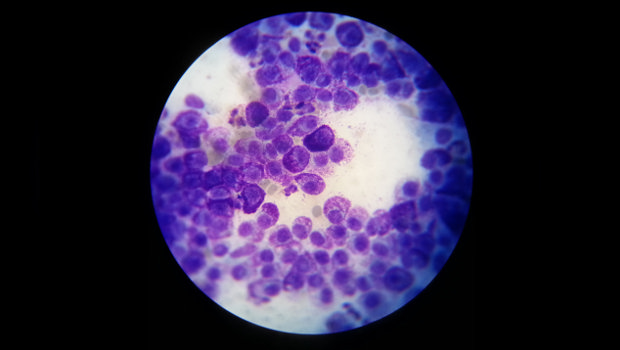
Cytology of a mast cell. Image credit: Rayya the Vet, via NIH Image Gallery.
Dr. Jennifer McClure reflects on evidence about mast cells as a key to chronic disease, providing new insights for physicians, researchers, and the public.
by Jennifer McClure, PhD, Group Health Research Institute Senior Investigator and Director of Research, Faculty & Development
I recently read Never Bet Against Occam: Mast Cell Activation Disease and the Modern Epidemics of Chronic Illness and Medical Complexity, by Dr. Lawrence Afrin. Dr. Afrin is a hematologist at the University of Minnesota, but he may more accurately be called a medical detective and pioneer in the identification and treatment of mast cell activation syndrome (MCAS). Dr. Afrin is one of many physicians and researchers who now believe MCAS may explain some of the most complex cases of chronic disease, not to mention the rising number of patients with chronic illness.
Never heard of MCAS? You’re not alone, which is what makes this story so incredible.
What is MCAS?
Doctors know that mast cells are part of the immune system, but they might not know about MCAS, which was only recently recognized as one of two forms of mast cell activation disease. The better-known form, mastocytosis, is very rare and results from too many mast cells. In contrast, people with MCAS have a normal number of mast cells, but those cells behave badly. In addition to responding to common allergens, in MCAS the mast cells can be hyper-responsive to otherwise non-threatening stimuli, even foods, smells, and physical or emotional stressors. We don’t yet know how common MCAS is, but preliminary research suggests it may affect one in six people (~17 percent).
Why is rogue mast cell activation bad?
When activated, mast cells release many chemicals (such as histamine, heparin, leukotrienes, cytokines, and many others). These chemicals directly or indirectly cause a host of responses in the body including (but not limited to) inflammation, pain, and slow wound healing. Chronic inflammation is as an important underlying cause of chronic disease, since prolonged inflammation can damage the body and is even implicated in some neuropsychiatric illness. By constantly causing inflammation and other reactions in the body, chronic mast cell activation can wreak havoc. And because mast cells are located throughout the body, this havoc can appear just about anywhere.
What should providers know about MCAS?
If Dr. Afrin and his colleagues are correct, MCAS should always be suspected in people with poorly explained chronic, multisystem disease, particularly when allergic symptoms or inflammation are involved. Dr. Afrin’s book also nicely illustrates how frustrating this condition is for patients and providers because MCAS can look different in each person and a patient’s symptoms can change over time as different organ systems are affected. It appears that MCAS is more prevalent in females than males (3:1).
What does the future hold for MCAS?
In time, we will learn more about the underlying cause of MCAS (current thinking attributes it to one or more genetic mutations), how to effectively manage the disease, and perhaps even how to cure it. In the meantime, Dr. Afrin and his colleagues want to raise awareness of MCAS among the medical community and patients living with chronic disease. With this awareness will come the necessary funding, research, and knowledge needed to help us reduce the pain and suffering experienced by those living with chronic disease due to MCAS.
What does this mean for GHRI?
If MCAS is as common as suggested, many people—including many Group Health members—could be affected. GHRI is well positioned to contribute to future studies of MCAS given the size of our patient population, our access to comprehensive medical records from primary and specialty care, and our leading scientists in epidemiology and chronic disease management.
I encourage physicians, scientists, and anyone interested in chronic disease to learn more about this exciting new area.
Suggested reading
Afrin, L. Never Bet Against Occam: Mast Cell Activation Disease and the Modern Epidemics of Chronic Illness and Medical Complexity. (2016). Sisters Media, Bethesda, MD.
Afrin L, Butterfield JH, Raithel M, and Molderings GJ. Often seen, rarely recognized: mast cell activation disease—a guide to diagnosis and therapeutic options. Annals of Medicine, 48(3):190-201.
Afrin L. (March 2016). A new era for an old cell: heightened appreciation of mast cell disease emerges. Translational Research. [Epub ahead of print].