Chronic Care Model change concepts
Chronic Care Model: Change Concepts
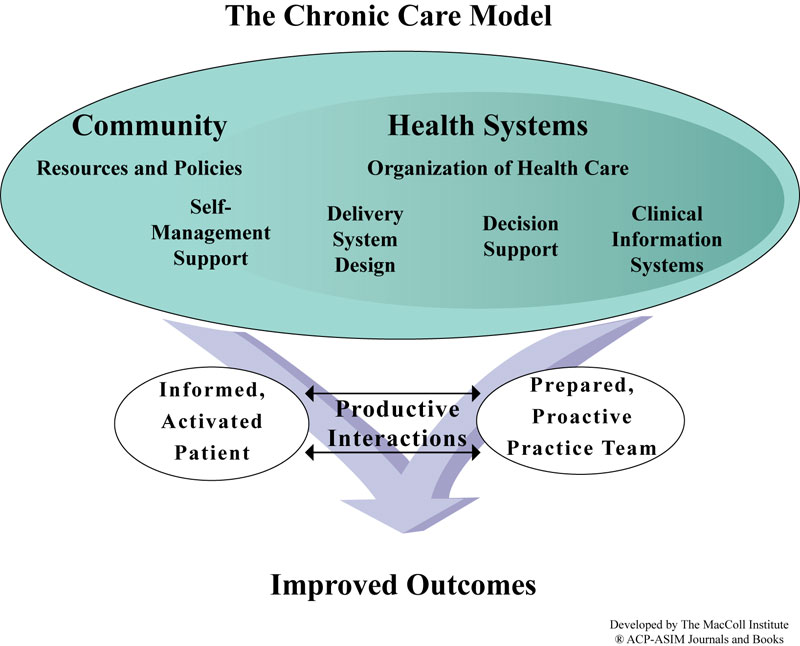
The Chronic Care Model identifies essential elements of a health care system that encourage high-quality chronic disease care: the community; the health system; self-management support; delivery system design; decision support, and clinical information systems. Within each of these elements, there are specific concepts (Change Concepts) that teams use to direct their improvement efforts. Change concepts are the principles by which care redesign processes are guided.
Health System: create an organization that provides safe, high quality care
A health system’s business plan reflects its commitment to apply the CCM across the organization. Clinician leaders are visible, dedicated members of the team.
- Visibly support improvement at all levels of the organization, beginning with the senior leader
- Promote effective improvement strategies aimed at comprehensive system change
- Encourage open and systematic handling of errors and quality problems to improve care
- Provide incentives based on quality of care
- Develop agreements that facilitate care coordination within and across organizations
The Community: mobilize community resources to meet needs of patients
Community resources, from school to government, non-profits and faith-based organization, bolster health systems efforts to keep chronically ill patients supported, involved and active.
- Encourage patients to participate in effective community programs
- Form partnerships with community organizations to support and develop interventions that fill gaps in needed services
- Advocate for policies that improve patient care
Self-Management Support: Empower and prepare patients to manage their health care
Patients are encouraged to set goals, identify barriers and challenges, and monitor their own conditions. A variety of tools and resources provide patients with visual reminders to manage their health.
- Emphasize the patient’s central role in managing his or her health
- Use effective self-management support strategies that include assessment (physician or self?), goal setting, action planning, problem-solving and follow-up
- Organize internal and community resources to provide ongoing self-management support to patients
Delivery System Design: Assure effective, efficient care and self-management support
Regular, proactive planned visits which incorporate patient goals help individuals maintain optimal health and allow health systems to better manage their resources. Visits often employ the skills of several team members.
- Define roles and distribute tasks among team members
- Use planned interactions to support evidence-based care
- Provide clinical case management services for complex patients
- Ensure regular follow-up by the care team
- Give care that patients understand and that agrees with their cultural background
Decision Support: Promote care consistent with scientific data and patient preferences
Clinicians have convenient access to the latest evidence-based guidelines for care for each chronic condition. Continual educational outreach to clinicians reinforces utilization of these standards.
- Embed evidence-based guidelines into daily clinical practice
- Share evidence-based guidelines and information with patients to encourage their participation
- Use proven provider education methods
- Integrate specialist expertise and primary care
Clinical Information Systems: Organize data to facilitate efficient and effective care
Health systems harness technology to provide clinicians with an inclusive list (registry) of patients with a given chronic disease. A registry provides the information necessary to monitor patient health status and reduce complications.
- Provide timely reminders for providers and patients
- Identify relevant subpopulations for proactive care
- Facilitate individual patient care planning
- Share information with patients and providers to coordinate care
- Monitor performance of practice team and care system
So What Does All This Mean?
Successful system change means you will redesign care within each of the six components of the CCM; it does not mean tweaking around the edges of an acute care system not capable of handling the needs of the chronically ill. You will be building a new system that works in concert with your acute care processes. You will accomplish this by testing the above change concepts and adapting them to your local environment. The remaining steps in this manual help focus where you can start making these changes.
Tools That Can Help
After learning more about the chronic care model, there are two things that may assist you in understanding how it directs system change:
- The Assessment of Chronic Illness Care (PDF) is a diagnostic survey that you and your team can complete together. The ACIC helps you identify that current state of your chronic care; what’s working and what is needed to achieve redesign in all components of the CCM.
- Curing the System: Stories of Change in Chronic Illnesss Care (PDF) is a report that provides concrete examples of teams that have redesigned their care based on the CCM. Some of the stories and the practices they represent may resonate with you and your team.
Using our materials in
your work
The MacColl Center encourages the
non-commercial use or adaptation of the materials we develop. With the exception of the Chronic Care Model image above, all other materials provided here are publicly available, free of cost and copyright protected.
contact us
Please email us at maccoll@kp.org for help finding additional tools from Improving Chronic Illness Care.
Our other websites
The MacColl Center's funding for Improving Chronic Illness Care ended in 2011, but our work to improve care with a patient-centered, team-based approach has continued. To access some of our more recent tools and resources, please visit these websites:
Assessments
- Assessment of Chronic Illness Care (ACIC)
- Patient Assessment of Chronic Illness Care (PACIC - 20 item)
- Patient Assessment of Chronic Illness Care (PACIC - original)
- Patient-centered Medical Home Assessment (PCMH-A)



