SPARC trial tools
 OUR TEAM & PATIENT STORIES
OUR TEAM & PATIENT STORIES
Our team
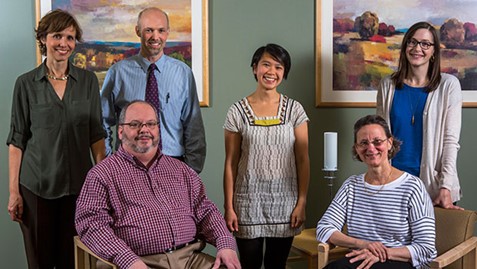
SPARC trial team members (front row) Larry Marx, MD; Kathy Bradley, MD, MPH; (back row) Paula Lozano, MD, MPH; Ryan Caldeiro, MD; Amy Lee, MPH; Rebecca Parrish, LICSW, MSW

SPARC trial team members (front row) Kathy Bradley, MD, MPH; Tory Gildred, LICSW, CDP; Ryan Caldeiro, MD; (back row) Paula Lozano, MD, MPH; Rebecca Phillips, MA; Evette Ludman, PhD; Amy Lee, MPH; and Julie Richards, PhD MPH
Research
Katharine Bradley, MD, MPH
Jennifer Bobb, PhD
Julie Richards, PhD, MPH
Joseph Glass, PhD, MSW
Paula Lozano, MD, MPH
Gwen Lapham, PhD, MPH, MSW
Emily Williams, PhD, MPH
Megan Addis, BA
Malia Oliver, BA
Rebecca Phillips, MA
Carol E. Achtmeyer, ARNP, MN
Evette Ludman, PhD
Clinical operational partners
Ryan Caldeiro, MD
Rebecca Parrish, LICSW, MSW
Amy K. Lee, MPH
Larry Marx, MD
Tori Gildred, LICSW, MSW, CDP
Patient and provider stories
Behavioral Health Integration (BHI) gave us the opportunity to identify and provide coordinated care for an urgent problem that we might not have recognized otherwise.
- Julia Sokoloff, Olympia Primary Care Physician
Behavioral Health Integration (BHI) changed the culture…it opened the door and made it okay for patients to talk about behavioral health concerns that they might not have felt comfortable initiating.
- Santino Telles, Northgate Medical Assistant
The Behavioral Health Integration (BHI) roll-out is the best I have seen in primary care. The teams were so engaged and supported.
- Mamatha Palanati, APIC
Inspired to take action: How BHI empowered an MA to step in and help a patient in crisis
Toni Dow, MA, a medical assistant at Kaiser Permanente Lynwood Medical Center, describes how she tapped into BHI's social work resources to get help for a distraught-looking patient who had come into the clinic to pick up a letter.
One of the best outcomes of behavioral health integration (BHI) is how it has empowered MAs as members of a patient's care team. That personal feeling of empowerment is what inspired me to take action one day when I noticed a distraught patient who had come into the Lynnwood clinic to pick up a letter for her work.
This patient, a woman in her 50s, asked me if the clinic had psychiatry services onsite. I immediately thought to connect the patient to our social worker, Heather Ford. While we waited, I took the patient aside and chatted with her for a while. I discovered that the patient had just learned some devastating news. She was in crisis and needed help.
The social worker was able to meet with her that same day.
As a result of BHI, our patient was able to go home that night feeling listened to. She left our clinic equipped with some new self-care strategies, coping skills, and a plan for further assistance. Because our clinic has a social worker on-site, I was able to connect the patient with the care she needed when she was in crisis. BHI makes it possible to get patients connected to care in one place at one time. It’s truly patient centered. I’m proud of the role I play in BHI each day, and I’m thankful that I felt empowered to step in and help this patient when she was in need.
Behavioral Health Integration: Empowered medical assistants are at the forefront
Northgate Medical Assistant (MA) Santino Telles, MAC, talks about the important role MAs play in BHI’s success — and how BHI has helped make his work more meaningful and rewarding.
When my fellow Northgate MAs and I first heard about behavioral health integration (BHI), we all thought, “Oh, more paperwork, more work for us.” But BHI is so much more than paperwork — it’s a chance to get closer to our patients and to make a real difference in their lives.
MAs are the first touch point in BHI. We are the first ones to see patients’ answers on the questionnaires, which ask about their feelings of depression and about their drinking and substance use. If a patient’s answers indicate that they’re having trouble with any of these things, we notify the social worker or the provider so that the patient can get the right care right away.
All the MAs at Northgate received training on how to engage patients in talking about sensitive topics like depression and unhealthy drinking since patients may have questions — and we learned that the key was to not stigmatize. So we don’t use words like “alcoholic” or “drug abuser.” Patients realize that we’re not judging them or asking them to admit to anything. We’re just talking about their behavioral health — and approaching drugs and alcohol use as part of that.
Most patients answer these questions honestly. Then we, the MAs, are able to respond in an objective way. We simply say, “This is what you’ve told us.” That lets patients know that they’re being heard instead of judged. I’ve been surprised by how rarely patients respond with, “It’s none of your business.” In fact, about 4 out of 10 will say, “Thank goodness you asked about this,” or “Thank you for caring.”
Saving and improving lives: How BHI provides care ‘on another level’
I realized pretty quickly after getting started with BHI that screening patients really didn’t take much more time. And it’s obvious that it has a positive impact. Since implementing BHI at Northgate, we’ve been able to identify and provide care for many more depressed and anxious patients. These are usually people who have learned to hide it pretty well. With social work and behavioral health services in the building, the initiative gives them quick access to help.
We once had a patient say, “I’m going to kill myself today.” And through social work and behavioral health upstairs we were able to provide appropriate follow-up care right away. It was great to see that particular patient walk through the door a couple weeks later. The patient is still anxious and still having some negative thoughts, but now they know we are here to help them. And they are on the road to a better managed life.
Another remarkable thing about BHI is how it helps us identify unhealthy alcohol use and gives us a new perspective on chronic disease management. For example, if we have a patient with diabetes, and we discover they’re depressed and drinking heavily … maybe that’s why they’re not checking their blood sugar or taking their meds. If we address their depression and unhealthy alcohol use, maybe they will take better care of their diabetes.
Overall, BHI lets patients know we’re on another level with how we provide care. We are reaching out to identify struggles they’re having that would probably have gone unnoticed. We’re letting them know that we can help them get through struggles — and that we’ll do so without stigmatizing or judging them.
‘I feel empowered’: How BHI has elevated the role of the MA
BHI has allowed MAs to take control and ownership of their part in the process of care. I love the fact that, as an MA, I am seen as important enough to be able to interact with patients on this level. It makes me feel like the doctors value my perspective and trust my judgment. My fellow MAs and I feel empowered, and we’re proud that we get to help bring behavioral health services to patients who need them — but who might not get them if not for us using our training and skills.
With this overall integration across Kaiser Permanente, MAs have been at the forefront. BHI gives us this feeling like, “This is my clinic. This is my patient.” It’s a beautiful thing to be a big part of somebody’s betterment. We see suicidal patients who walk back in a week later, and you see that they’re doing better. It’s rewarding on such a deep level. BHI even helps in my personal life, too. It reminds me to slow down and check in with myself.
For all the MAs who read this, I would say this: Love your job, have fun with it, and know that you’re important. And know that you as the MA are the spearhead of BHI, the initial point of contact for patients. Be proud of this work and make it your own.
From irritated to engaged: How a 'no-contact' letter opened the door to helping a patient change unhealthy drinking habits
Kathleen Cullen, LICSW, a social worker at Kaiser Permanente Riverfront and Veradale Medical Centers, describes how sending a “no-contact” letter prompted an irritated patient to call her — and how she used the opportunity to engage him in care for unhealthy drinking.
As part of behavioral health integration (BHI), my fellow social workers and I routinely call patients recently diagnosed with a substance use disorder who appear on a report. After a few unsuccessful attempts, I’ll send a “no-contact” letter — explaining to the patient that I’m hoping to speak with them and requesting a call back.
When patients do contact me after receiving the letter, it’s hard to know what to expect. I remember one patient in particular who was irritated that I’d sent the letter. We started talking, and I explained that I was trying to reach him because I thought I could help him with his anxiety. It appeared he was using alcohol to try to cope with it, and that didn’t seem to be working well as he was still anxious. I explained that maybe if he engaged in therapy he could then cut down on his drinking, which would help him with his overall health care goals.
At first, he was defensive and gave me many reasons for why he drank so much. But I kept talking with him in a non-judgmental way, and he finally opened up — saying that he knew he drank way too much but couldn’t seem to stop. He even said he was interested in getting help … but that he needed time to think more about it.
As we hung up, he said, “Wow, I didn’t expect this to be a good conversation. Thank you.” He agreed to let me call him in a week if I didn’t hear from him first. Imagine my surprise when my phone rang a few minutes later and it was him — calling back to schedule an appointment with me.
When he came in for that appointment, I engaged him in learning some alternative skills to manage anxiety. With that, he was able to significantly reduce his alcohol intake. After several weeks he decided that maybe alcohol was not something he needed at all — and that, for him, drinking did more harm than good.
And to think this all started with the patient being annoyed by the letter I sent. It just goes to show that you never know what will work to get your foot in the door. But once you have a chance to engage the patient in talking about how you can help them, anything is possible.
Providing the right care at the right time for a patient in need
Julia Sokoloff, MD, a primary care physician at Kaiser Permanente Olympia Medical Center, describes how BHI allowed her to identify and help a potentially suicidal patient.
My patient, a middle-aged woman, had come in for a simple wart removal. As part of our standard behavioral health screening for behavioral health integration (BHI), we discovered that she was acutely suicidal. She left the visit with a crisis plan, a prescription for antidepressants, and follow-up visits already scheduled. We might not have known this patient needed help if we hadn’t used the new BHI screening tool.
My MA, Linda Phan, administered the screening tool during rooming and saw that the patient screened positive for depression, so she asked the patient to fill out the rest of the PHQ-9. The patient had answered all the questions by the time I came in to meet with her. I was surprised to find that her score totaled 24 and that she had been having thoughts of harming herself.
I asked the patient how she was doing, and we talked about her depression and her medication options. When I asked her if she would be interested in talking further with a member of my team, she said “yes.” I paged the social workers, and Mithila Pathare, LICSW, arrived immediately. We completed a warm handoff, and I left to see my next patient.
The social worker assessed the patient’s suicidality, developed a crisis plan with her, and engaged her in shared decision-making about her options. The patient decided that she was interested in trying medications for her depression. When I checked back with them later, the patient and I spoke more about medication options and I started her on an antidepressant. The patient left with a plan in place and with follow-up appointments scheduled with me and with the social worker. On the way out, she told us how grateful she was for the care she had received.
I, too, am grateful that BHI gave us the opportunity to identify and provide coordinated care for an urgent problem that we might not have recognized otherwise. That’s patient-centered care at its best.
How a skeptical provider put BHI to the test and helped a patient with previously unrecognized alcohol use disorder
Concerned about adding to his workload, Mark Spee, MD, decided to “test” BHI. The result? Great care for a patient with a critically important problem that had gone unnoticed.
I have to admit I was skeptical about behavioral health integration (BHI) at first because I thought it would create more work for me and other busy primary care physicians. But soon after my team started using the standard screening tool, something happened that made me realize how practical and valuable it is.
Thanks to a proactive follow up, a patient with alcohol use disorder is on the path to better health
Rebecca Parrish, MSW, LICSW, a social worker at Kaiser Permanente Burien Medical Center, tells the story of how she identified a patient with alcohol use disorder (AUD) and engaged him in a plan to stop drinking.
One important part of the expanded role social workers play as integrated behavioral health specialists is a reporting workbench in Epic that automatically notifies me when a patient is seen for care related to an alcohol or substance use disorder diagnosis. I remember one patient in particular who had sustained a C4 neck fracture after a very bad fall while intoxicated. He was sent home from urgent care (UC) with a neck brace and some encouragement to not drink.
I saw this patient on the Epic workbench and called to see how he was doing and noticed his speech was slurred. I clarified that, although he told his UC providers that he was drinking 3 drinks a night, his intake indicated it was actually more like 7 to 10 standard drinks. I also found out that he had not had a drink since his UC visit 2days prior. Concerned about his slurred speech and the possibility of withdrawal symptoms, I contacted his primary care provider (PCP), who called the patient to see how he was doing. Based on our assessment, his doctor advised him to go to the emergency department (ED) for an evaluation to assess possible cranial nerve dysfunction due to the neck fracture or alcohol withdrawal symptoms.
I followed up with another phone call to the patient to see how he was doing. We talked about his previous and current drinking and discovered that he had no medications to help him detox. I was also able to speak with the patient’s daughter, who was concerned about her father’s pain and trying to coordinate his care. She expressed how grateful she was for our phone calls and our advice to take her father to the ED that day. We also scheduled him to see his PCP the very next day for follow-up care on his neck fracture and a prescription for medications to manage his pain and withdrawal symptoms.
I met with the patient after his PCP visit, and we reviewed options for care and worked together on a continued abstinence plan. I shared some resources with him and entered a referral for a chemical dependency assessment. We also talked about his motivation for changing his alcohol use and how medications for AUD might help.
This patient ended up declining outpatient chemical dependency services but has had regular follow-up with me and his PCP ever since his fall and our initial outreach to him. Without the Epic workbench, I never would have known about this patient. The best part: He dropped in recently to let me know that it has been more than 8 months since he’s had a drink and that he’s doing great.
How BHI helped a patient recognize and engage in treatment for depression
Angela Garza McWethy, MSW, LICSW, a behavioral health specialist at Kaiser Permanente Northgate Medical Center, tells the story of how BHI screening and treatment helped turn things around for a patient who was depressed but had been focused on caring for his wife with dementia.
At Northgate Medical Center, we implemented behavioral health integration (BHI) in 2 of our 4 clusters in September 2015. Since then, I’ve had great patient feedback about the screening and system that we have in place to support patient care.
I met with a middle-aged man who had many different chronic conditions, including type II diabetes, sleep apnea, spinal stenosis, and severe obesity. On top of this, he had been experiencing severe depression since his wife, diagnosed with dementia 10 years prior, was moved to a nursing home for long-term care. He came into our clinic and, based on his screening, his doctor thought that he could benefit from short-term therapy with me. He scored an 18 on the PHQ-9, which met the criteria for major depressive disorder (moderately severe).
This is how we got connected to start treating his depressive symptoms for the first time. He had been a caregiver for his wife for so long that taking care of himself was not in his scope of vision. Meeting with me was the first time he’d tried to tackle this on his own.
We started working on coping skills and goal setting during our first appointment to help him with feeling better overall. During each session, we would build from skills learned in the prior session and continue setting goals that made him feel more confident in his ability to move forward in his life.
During our last session, he scored a 9 on the PHQ-9 (mild) and reported feeling much better in his daily life and what he’s doing now that he’s retired. He was thankful that this was something we addressed and that we offered to give him the extra push to get started in short-term treatment.
Positive outcomes like this are what we hope to see in many of our patients. It starts with addressing depression in a medical visit and ends with patient engagement in treatment. Without the screening tool, this patient would not have been asked key questions that got him thinking about improving his depression in the first place.
From caring for a cold to a potentially life-saving intervention
Kara Rice, LICSW, a social worker at Kaiser Permanente Olympia Medical Center, describes how BHI prompted immediate action to help an acutely suicidal patient who had come in for a cold.
One of the amazing things about behavioral health integration (BHI) is that we get a chance to help people immediately — and sometimes being able to act quickly can make all the difference. This was especially true in the case of a 24-year-old patient who had come to the clinic to be seen for a cold. Because of our new behavioral health screening standards, we were alerted to the fact that this young man wasn’t just suffering from a cold — he was acutely suicidal.
I was paged to come talk with this patient after he scored high on our behavioral health screening tools. I learned that, not only was this patient severely depressed, he had attempted suicide twice in the past 2 weeks. In fact, the day before I met with him, he had played Russian roulette with his father’s revolver—attempting to shoot himself in the head 3 times.
I completed the Columbia suicide risk assessment with him, and he screened very high. Next, we talked about his immediate safety, and I discovered that he had limited outside supports. Because his safety couldn’t be guaranteed if he went home, we talked about inpatient psychiatric treatment, which he agreed was a good idea.
So I asked his primary care doctor to place lab orders and then walked the patient to urgent care, where they were happy to monitor him until a bed became available. Next, I coordinated his follow-up care, and the patient was authorized for psychiatric admission within 4hours. I also talked with his parents, who waited with him in urgent care and later drove him to his psychiatric placement.
Thanks to BHI, we had systems in place that let us know this young man was in immediate danger, and we were able to intervene and help him right away. Who knows what might have happened if he had come and gone and only been treated for his cold? This is world-class BHI, and I’m so proud of the work we’re doing to help patients in need.
With encouragement, medication, and time, a patient with AUD is drinking half as much as he used to
Mithila Pathare, a social worker at Kaiser Permanente Olympia Medical Center, explains how she worked with a patient over time to engage him in care for an alcohol use disorder (AUD). With the help of medication, he has successfully cut his drinking in half.
When I started working with this 48-year-old patient at the first meeting, he was interested in changing providers. He had talked with his current provider about his alcohol use. But he wasn’t interested in going to Alcoholic Anonymous meetings or going to an alcohol treatment program, which was the only course of treatment his provider recommended.
He also wasn’t interested in trying medication and said he wasn’t experiencing any cravings. At first, I wasn’t sure whether he really wanted to cut back on his drinking. He had missed quite a few appointments, and I wasn’t sure he wanted to work with me. But when I asked him if he thought therapy with me was helpful, he said it was.
So I kept working with him and ultimately learned an important lesson: Sometimes it just takes time.
After 2 sessions of talking about how medication could help him, he decided to give it a try. His new provider prescribed naltrexone, and the patient picked up his prescription the day before Thanksgiving. On Thanksgiving Day, he drank less than his family — which was quite different from the norm.
I’ve met with him 6 times now, and he’s made some big changes. He has cut his daily intake down from 6 beers to 3. Initially, he had said that cravings weren’t a problem for him. But now he talks about how the medication has really helped ease his cravings. He even said that drinking less feels like the “fog has lifted off his head.”
Understanding that patients sometimes need their own time to change is the biggest lesson I’ve learned through our work to address AUD in primary care. As social workers we need to think about sowing seeds in patients’ minds; when patients are ready to make changes they will in their own time.


