James D. Ralston, MD, MPH
Biography
James Ralston MD, MPH, is an internal medicine physician and senior investigator in health services and health informatics. His research mission is improving the health and care of patients living with common ongoing illnesses. His current areas of emphasis include understanding and honoring the priorities of patients living with multiple chronic conditions.
Dr. Ralston’s research focuses on developing and evaluating communication technologies that foster continuous care and a closer connection between patients and primary care teams. His commitment to finding effective ways to redesign care spans all stages of research, from project development to complete translation of results into clinical practice.
Examples of Dr. Ralston’s research projects include:
- The Valuing Important Things in Active Lives (VITAL) study to improve care for people with multiple chronic conditions including diabetes, heart disease, and arthritis. VITAL uses participatory design methods with patients and providers to design and evaluate interactive care plans.
- The Seeing Priorities study to build and test a single, trusted tool for individuals with multiple chronic conditions that illuminates connections between personal values and chronic illness management. The tool helps visualize, track, and share what matters most for self-management and care.
- Understanding and addressing differences in patient use of online health care services that could lead to care disparities.
- Testing online care management of blood sugar control using an electronic health record shared with patients with type 2 diabetes. Control improved in patients receiving online care management in addition to usual care.
- Validating and evaluating a clinical tool to identify patients with type 2 diabetes at risk of severe low blood sugar. This national collaboration uses Kaiser Permanente and Veterans Administration electronic health record data and machine learning methods.
- Testing innovative engagement methods such as photos taken by study participants to document their values to ensure that patient priorities guide self-management plans and clinical care.
- Working with primary care teams and clinics in rural and underserved areas to improve the care of their patients with chronic conditions.
Dr. Ralston is also a University of Washington affiliate professor in health services and biomedical informatics, where he serves on the committees of PhD and master’s degree students.
Research interests and experience
-
Health Informatics
eHealth; hypertension; diabetes
-
Chronic Illness Management
Health informatics; hypertension; diabetes; health behaviors; multiple chronic conditions
-
Behavior Change
Self-management support
-
Health Services & Economics
Health care disparities
Recent publications
Arsand E, Tufano JT, Ralston JD, Hjortdahl P. Designing mobile dietary management support technologies for people with diabetes. J Telemed Telecare. 2008;14(7):329-32. PubMed
Green BB, Ralston JD, Fishman PA, Catz SL, Cook A, Carlson J, Tyll L, Carrell D, Thompson RS. Electronic communications and home blood pressure monitoring (e-BP) study: design, delivery, and evaluation framework. Contemp Clin Trials. 2008;29(3):376-95. Epub 2007 Sep 26. PubMed
Ralston JD, Carrell D, Reid R, Anderson M, Moran M, Hereford J. Patient web services integrated with a shared medical record: patient use and satisfaction. J Am Med Inform Assoc. 2007;14(6):798-806. Epub 2007 Aug 21. PubMed
Carrell D, Ralston J. Variation in adoption rates of a patient web portal with a shared medical record by age, gender, and morbidity level. AMIA Annu Symp Proc. 2006;871. PubMed
Ralston J, Carrell D. Use and satisfaction of a patient Web portal with a shared medical record between patients and providers. AMIA Annu Symp Proc. 2006;1070. PubMed
Greene SM, Larson EB, Boudreau DM, Johnson K, Ralston J, Reid R, Fishman P. The Coordinated Clinical Studies Network: a multidisciplinary alliance to facilitate research and improve care. The Permanente Journal. 2005;95(4):33-5. PubMed
Ralston JD, Larson EB. Crossing to safety: transforming healthcare organizations for patient safety. J Postgrad Med. 2005;51(1):61-7. PubMed
Carrell D, Ralston J. Messages, strands and threads: measuring use of electronic patient-provider messaging. AMIA Annu Symp Proc. 2005;913. PubMed
Hislop TG, Teh C, Lai A, Ralston JD, Shu J, Taylor VM. Pap screening and knowledge of risk factors for cervical cancer in Chinese women in British Columbia, Canada. Ethn Health. 2004;9(3):267-81. PubMed
Ralston JD, Revere D, Robins LS, Goldberg HI. Patients' experience with a diabetes support programme based on an interactive electronic medical record: qualitative study. BMJ. 2004;328(7449):1159. PubMed
News

LHS E-STAR training program selects 3 new scholars
Trainees will lead learning health system research at Kaiser Permanente Washington and VA Puget Sound.
Research

Identifying patients in need of social support services
Kaiser Permanente researchers develop predictive model to help adults with multiple health conditions.
News

Training scientists as partners in transforming primary care
Newly funded center will elevate equity and community in learning health system research.
Research
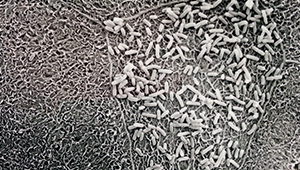
Resistant E. coli rises despite drop in ciprofloxacin use
Community circulation of ciprofloxacin-resistant E. coli increased after 6-year reduction in antibiotic prescriptions
Research

Some adolescents are more likely to use patient portal than others
A new study aims to understand trends in digital care communication among teens.



